Blackford Middleton, MD, MPH, MSc
Aided and abetted by several AI’s Deep Research.
1. Executive Summary
Overview: This report evaluates the hypothesis that the impact of Artificial Intelligence (AI) in healthcare—spanning improvements in quality of care, cost reduction, provider and patient experience, and population health—varies significantly based on the state of IT/internet infrastructure and prevailing healthcare payment models. AI holds immense promise for transforming healthcare delivery globally 1, driven by rapid technological advancements and substantial investment.4 However, its adoption and realized benefits are demonstrably uneven across different systems and regions.3
Key Findings: The analysis confirms the central hypothesis, albeit with important nuances. Both digital infrastructure (encompassing data readiness, interoperability, digital maturity, and connectivity) and healthcare payment models (determining incentive alignment and return on investment viability) critically modulate AI's effects. Robust infrastructure is a necessary foundation, enabling the data flow and integration required for sophisticated AI tools. Aligned payment models, particularly value-based care (VBC), provide the incentives to leverage AI for improving outcomes and efficiency.9 However, these are not the sole determinants. Factors such as effective governance, regulatory clarity, clinician and patient trust, ethical considerations, and workforce readiness are also vital for successful AI implementation and impact, sometimes irrespective of infrastructure or payment structure.8
Top Discerning Factors: The analysis identifies five critical factors that differentiate the potential and realized impact of AI in healthcare globally:
Digital Infrastructure Maturity: The foundational technological capacity, including connectivity and EHR adoption.
Data Governance, Interoperability & Privacy Frameworks: The rules and standards governing data access, sharing, and ethical use.
AI Talent Pool & Digital Skills: The availability of human expertise to develop, deploy, and utilize AI.
Investment & Funding Environment: The level of financial resources dedicated to AI research, development, and adoption in healthcare.
Payment System Alignment & VBC Adoption: The degree to which payment models incentivize the use of AI for value creation (improved outcomes and efficiency).
Country Rankings: This report presents Top 10 country rankings for each of these five factors, derived from relevant global indices and comparative data. These rankings illustrate the significant global variations in preparedness to harness AI effectively in the healthcare sector.
Strategic Implications: Realizing the full potential of AI in healthcare requires a multi-faceted approach. Stakeholders must address infrastructure gaps, accelerate payment reform towards value-based models, establish robust governance and ethical guidelines, invest in workforce development, and foster trust through transparency and proven real-world value. Integrated national strategies are crucial for navigating this complex landscape effectively.
2. Introduction
The Promise and Challenge of AI in Healthcare: Artificial Intelligence (AI) stands poised as a transformative force in healthcare, offering unprecedented opportunities to enhance diagnostics, personalize treatments, accelerate drug discovery, streamline administrative processes, and improve overall population health.1 Driven by exponential growth in health data, computational power, and algorithmic sophistication, AI technologies are rapidly evolving.4 Significant investments are flowing into the sector, reflecting the high expectations for AI to address persistent challenges like rising costs, workforce shortages, and variations in care quality.4 AI allows for a fundamental shift towards data-driven discovery and decision-making, potentially moving health systems from reactive to proactive and even predictive models of care.1
The Variability Problem: Despite this immense potential and growing enthusiasm, the diffusion and impact of AI technologies in healthcare practice have been notably uneven.7 While some applications show promise in controlled settings or specific domains, widespread adoption and transformative effects remain limited in many parts of the world.3 This variability raises a critical question: what factors determine the success and impact of AI in different healthcare contexts? This report investigates the central hypothesis that this variation is significantly influenced by the interplay of two crucial contextual factors: the maturity and nature of a healthcare system's IT and internet infrastructure, and the structure of its healthcare payment models.
Report Objectives and Structure: The primary objective of this report is to rigorously evaluate the aforementioned hypothesis. It undertakes this by:
Defining the scope of AI applications currently deployed or under development across key healthcare domains.
Assessing the general impact of AI on quality of care, cost, provider experience, patient experience, and population health, based on available evidence.
Analyzing how specific elements of IT and internet infrastructure (including Electronic Health Record (EHR) adoption, data interoperability standards like FHIR, broadband access, cybersecurity, and data governance) enable or hinder AI deployment and effectiveness.
Investigating the relationship between different healthcare payment models (e.g., Fee-for-Service (FFS), Value-Based Care (VBC), capitation) and the incentives or barriers they create for AI adoption and impact.
Synthesizing these findings to determine whether the evidence confirms that AI's impact varies significantly based on the combination of infrastructure and payment models, seeking comparative analyses where possible.
Identifying the top five global factors that most significantly differentiate AI's potential or realized impact in healthcare.
Providing ranked lists of the top 10 countries for each of these factors, based on relevant global indices and datasets.
The report is structured to first establish the landscape of AI applications and their general impact, then delve into the specific roles of infrastructure and payment models, evaluate the core hypothesis based on this analysis, identify key global differentiators, present country rankings, and finally, offer conclusions and strategic recommendations for stakeholders navigating the integration of AI into healthcare.
3. The Expanding Role of AI Across Healthcare Domains
Introduction: AI is rapidly moving beyond theoretical potential to practical application across a multitude of healthcare domains.1 Its ability to process vast datasets, identify complex patterns, and automate tasks is reshaping clinical practice, research, administration, and patient interaction.1 This transformation is underpinned by a fundamental shift towards data-driven discovery and decision-making, leveraging diverse data sources from genomics to real-world evidence captured by wearables and EHRs.1 The following sections explore the key areas where AI is making inroads and the evidence supporting its impact.
3.1 Diagnostics and Clinical Decision Support:
Applications: One of the most prominent areas for AI in healthcare is in augmenting diagnostic capabilities and providing clinical decision support (CDS).24 AI algorithms excel at analyzing medical images, including CT scans, MRIs, and X-rays, to detect anomalies indicative of various conditions.4 Applications span radiology (e.g., detecting fractures 22, tumors 25, pulmonary nodules 9), pathology (identifying cancerous cells 25), cardiology (predicting heart disease risk 25, improving diagnosis in cardiovascular cases 24), dermatology (recognizing skin conditions 25), ophthalmology (detecting diabetic retinopathy), and neurology (interpreting brain scans for stroke 22 or epilepsy lesions 22). Beyond imaging, AI is applied to genomic data analysis for precision medicine, helping to identify disease risks and tailor treatments.1 Predictive diagnostics use patient data to forecast disease progression 4, while CDS systems integrate various data points to assist clinicians in diagnostic reasoning and treatment planning.6
Impact Evidence (Quality): Numerous studies demonstrate AI's potential to enhance diagnostic accuracy and speed.4 In some specific, pattern-recognition tasks, AI can match or even exceed the performance of human experts.22 For example, studies have reported AI improving diagnostic accuracy in cardiovascular and diabetic cases by 20-30% 24, increasing breast cancer detection by 17.6% in mammography screening 27, and successfully identifying 64% of epilepsy brain lesions previously missed by radiologists.22 AI-backed diagnostic support has also been linked to a reduction in diagnostic errors by up to 30% in complex cases 24, which is significant given that diagnostic errors contribute substantially to adverse patient events.24 However, the impact is not uniformly positive or straightforward. One study found that while ChatGPT performed well independently on diagnostic reasoning tasks, providing physicians access to it did not significantly improve their clinical reasoning scores, although it did speed up case assessments.29 This highlights the importance of human oversight and the need for AI to be effectively integrated into the clinical thought process, not just used as a standalone tool.22
The "Augmentation, Not Replacement" Paradigm: A consistent theme emerging from the research and expert commentary is that AI should be viewed as a powerful tool to augment human capabilities, not replace clinicians.3 AI's strengths lie in its ability to analyze massive datasets rapidly and identify subtle patterns that might escape human detection, potentially mitigating fatigue or cognitive biases.25 Examples include processing millions of medical images faster than radiologists 32 or analyzing complex genomic data.27 However, human clinicians remain essential for interpreting AI findings within the broader clinical context, exercising ethical judgment, managing uncertainty, communicating with empathy, and making final shared decisions with patients.25 Studies showing improved accuracy alongside findings that AI doesn't necessarily improve the underlying reasoning process 29 reinforce this view: AI assists primarily with data processing and pattern recognition, providing valuable input for the clinician's interpretation. Therefore, successful implementation hinges on seamless integration into clinical workflows 8 and building clinician trust through transparency, validation, and education.11
3.2 Drug Discovery and Development:
Applications: The pharmaceutical industry is increasingly leveraging AI to revolutionize the lengthy and costly process of drug discovery and development.1 AI algorithms analyze vast datasets (genomics, proteomics, chemical structures) to accelerate the identification and validation of novel drug targets.1 They predict drug-target interactions and optimize molecular compounds for desired properties, facilitating the design of more effective therapies.1 Advanced techniques like deep learning, including graph neural networks, are significantly speeding up processes like predicting protein-ligand binding affinities.1 Beyond discovery, AI streamlines clinical trials by optimizing design, improving patient recruitment through analysis of EHRs and RWD, predicting trial outcomes, and enabling real-time monitoring.1 AI also assists in formulation development, predicting the effects of different ingredients and manufacturing processes.4
Impact Evidence (Quality, Cost): The primary impact of AI in this domain is the potential for significant efficiency gains, reducing the time and substantial costs traditionally associated with bringing a new drug to market.3 By improving target identification, optimizing candidates early, and accelerating clinical trials, AI promises to make R&D more productive.1 This increased efficiency can lead to the development of more efficacious therapies designed with a deeper understanding of molecular mechanisms.1 Evidence also points to improved quality in specific areas, such as a reported 40% increase in the accuracy of predicting drug reactions, which could reduce adverse events.24
Data as the Bottleneck/Enabler: The successful application of AI in drug discovery and development is fundamentally dependent on the availability and quality of large-scale, diverse, and well-structured biomedical data.1 AI models, particularly complex ones like deep learning networks, require massive datasets encompassing genomics, proteomics, chemical structures, clinical trial results, and real-world data (RWD) to learn intricate patterns and make reliable predictions.1 The exponential growth in such biomedical data is a key driver enabling AI's potential in this field.4 Conversely, significant barriers arise from data fragmentation across different silos, lack of standardization, poor data quality, and difficulties in accessing data due to privacy regulations or proprietary concerns.3 Therefore, advancements in AI for pharmaceutical R&D are inextricably linked to progress in building robust data infrastructure, promoting data sharing policies 17, ensuring data quality, and adopting interoperability standards 35 that facilitate the aggregation and analysis of these critical datasets.
3.3 Administrative Tasks and Operational Efficiency:
Applications: A major area of AI adoption involves automating the numerous administrative tasks that consume significant resources in healthcare.23 AI technologies, including Robotic Process Automation (RPA), Natural Language Processing (NLP), and Generative AI (GenAI), are being applied to streamline workflows such as appointment scheduling and reminders 38, patient registration and data entry 37, billing and coding 15, insurance claims processing and prior authorization 23, and clinical documentation.22 AI-powered scribes, for instance, can listen to patient encounters and automatically generate clinical notes 27, while intelligent coding tools analyze clinical text to assign appropriate billing codes.39 AI is also used for optimizing resource allocation, managing supply chains, and predicting staffing needs.4
Impact Evidence (Cost, Provider Experience): The potential for cost savings through administrative automation is substantial. Administrative costs account for a large portion of healthcare spending (nearly 25% in the US 37), and AI is projected to save the industry hundreds of billions annually through efficiency gains and reduced manual labor.33 Specific examples include AI identifying billions in fraudulent claims 33 and optimizing operating room supply costs.38 Automation reduces operational overhead 15, improves process speed and accuracy 15, and minimizes costly human errors in tasks like billing and coding.6 Equally important is the impact on the provider experience. By reducing the burden of administrative tasks, particularly documentation which can consume hours of a physician's day, AI can free up clinician time to focus on patient care.27 Studies on AI scribes report physicians saving approximately an hour per day on keyboard tasks.27 This reduction in administrative workload is linked to decreased clinician burnout and stress 27 and measurable improvements in job satisfaction.42 The high interest from healthcare leaders in adopting AI for administrative efficiency reflects these potential benefits.37
Administrative AI as a Gateway Technology: The significant focus on administrative applications suggests they often serve as a practical and strategic entry point for AI adoption within healthcare organizations.31 Several factors contribute to this. Firstly, administrative processes are frequently repetitive, rule-based, and generate substantial data volumes, making them well-suited for automation technologies like RPA and ML.23 Secondly, the return on investment (ROI) for administrative AI can often be more clearly defined and quantified through metrics like time savings, error reduction, and direct cost cuts, compared to the more complex validation required for clinical AI.10 Thirdly, these applications generally involve lower direct risks to patient safety than diagnostic or treatment algorithms, reducing initial implementation barriers.31 Fourthly, addressing the heavy administrative burden is a major priority for clinicians suffering from burnout, making them potentially more receptive to tools that alleviate this pressure.27 Successfully implementing AI for administrative tasks can build organizational expertise, foster familiarity with AI technologies, and cultivate trust, thereby paving the way for tackling more complex and potentially higher-risk clinical AI applications in the future.31
3.4 Patient Monitoring and Engagement:
Applications: AI is increasingly used to enhance patient monitoring and engagement outside traditional clinical settings. Real-time data from wearable devices and EHRs can be analyzed by AI to monitor patient conditions and predict adverse events.1 AI enables personalized communication, sending tailored appointment reminders, medication adherence prompts, and health education materials.23 Virtual health assistants and chatbots, powered by AI (including NLP and GenAI), provide 24/7 support for tasks like symptom checking, triage, appointment scheduling, answering patient questions, and even offering mental health support.22 AI algorithms can also analyze patient data to identify individuals at risk of non-adherence to treatment plans 56 and help clinicians tailor care plans based on individual history, genetics, and lifestyle factors.23
Impact Evidence (Patient Experience, Quality, Cost): Evidence suggests AI can significantly improve the patient experience by offering more personalized interactions 23, increasing convenience and accessibility of information and support 22, and empowering patients to take a more active role in their health.55 Improved engagement through personalized reminders and support can lead to better treatment adherence.55 Clinically, AI-driven monitoring and engagement can contribute to better outcomes, such as reduced hospital readmissions (e.g., by 15-20% for chronic conditions 24, 30% reported for Huma platform 22) and faster emergency response times.24 These improvements can also translate into cost savings by preventing complications and reducing hospitalizations.41
Balancing Personalization with Privacy and Equity: The power of AI in delivering personalized patient care and engagement 23 is intrinsically linked to its ability to access and analyze vast amounts of sensitive patient data. This reliance raises critical considerations regarding data privacy and health equity.23 Effective personalization often requires integrating data beyond clinical records, potentially including lifestyle information, genetics, and even socioeconomic indicators derived from housing data.22 The collection, storage, and use of such comprehensive and sensitive data necessitate extremely robust data protection frameworks (like HIPAA and GDPR), transparent policies, and explicit patient consent.34 Furthermore, there is a significant risk that AI algorithms trained on historically biased datasets could inadvertently perpetuate or even amplify existing health disparities affecting underrepresented populations.7 Access itself poses an equity challenge; many AI-driven engagement tools rely on patient access to technologies like smartphones, wearable sensors, and reliable broadband internet, potentially widening the digital divide for those in rural areas or lower socioeconomic groups.3 Therefore, realizing the benefits of AI-powered patient engagement requires a deliberate focus on ethical data governance, algorithmic fairness auditing, ensuring data representativeness, and implementing strategies to guarantee equitable access to these technologies for all populations.
3.5 Population Health Management:
Applications: AI offers powerful tools for managing the health of entire populations.47 Its analytical capabilities are employed for enhanced disease surveillance, identifying patterns and predicting outbreaks of infectious diseases like COVID-19 or influenza.3 AI algorithms analyze large datasets, including EHRs, demographic data, and potentially social determinants of health (SDoH), to identify individuals or communities at high risk for specific conditions or adverse outcomes.22 This allows for targeted interventions and optimized allocation of public health resources.28 AI can help understand the complex interplay of factors influencing health outcomes, including SDoH identified through non-traditional data sources like housing data or social media analysis.22 Examples include AI models predicting malaria outbreaks in Liberia 18 or identifying patients' socioeconomic situations to inform care provision.22
Impact Evidence (Population Health, Cost, Quality): AI has demonstrated its value in improving the timeliness and accuracy of public health surveillance and outbreak prediction.28 This enables more proactive and targeted public health interventions, moving away from reactive responses.18 By identifying high-risk groups early and facilitating preventive measures, AI has the potential to improve population-level health outcomes and reduce health disparities.45 Furthermore, by optimizing the allocation of limited public health resources (staffing, supplies, interventions) based on predicted needs, AI can contribute to significant cost savings and increased efficiency in public health operations.18
Population Health AI Requires Cross-Sector Data Integration and Governance: To be truly effective, AI applications in population health management necessitate the integration of highly diverse data sources that extend far beyond traditional clinical records, coupled with robust governance frameworks.3 Population health is shaped by a complex web of clinical, social, economic, and environmental factors.22 AI models aiming to understand and predict population health trends need access to data reflecting this complexity, potentially including EHRs, public health registries, demographic data, environmental sensor data, socioeconomic indicators, and even anonymized data from social media or commercial sources.45 Aggregating and analyzing such disparate datasets presents substantial technical hurdles related to data standards and interoperability, as well as significant governance challenges concerning data privacy, security, ownership, and ethical use.3 Building and maintaining public trust is paramount when utilizing sensitive population-level data, demanding transparency in how AI models work and strong ethical oversight mechanisms.3 Consequently, successful and responsible AI initiatives in population health depend heavily on the existence of mature, interoperable data ecosystems, clear data sharing agreements, and collaborative governance structures that involve public health agencies, healthcare providers, researchers, and potentially community representatives.67
4. IT & Internet Infrastructure: The Digital Foundation for Healthcare AI
Introduction: The effective deployment and scaling of AI in healthcare are widely understood to depend critically on a robust underlying digital infrastructure.3 This foundation enables the collection, storage, transmission, and processing of the vast amounts of data that fuel AI algorithms and allows AI tools to be integrated into clinical and administrative workflows. Key components of this infrastructure include the prevalence and sophistication of Electronic Health Records (EHRs), the degree of data interoperability facilitated by standards like Fast Healthcare Interoperability Resources (FHIR), the availability and quality of broadband internet access, the maturity of data governance and quality assurance practices, the strength of cybersecurity measures, and the overall digital readiness of the healthcare system and its workforce.
4.1 The Role of Foundational Elements:
EHR Adoption & Data Digitization: The widespread adoption of EHR systems is a fundamental prerequisite for leveraging AI in healthcare, as these systems capture the clinical data—patient histories, diagnoses, treatments, lab results, notes—that serve as the primary input for many AI models.1 The transition from paper records to digital formats creates the necessary substrate for AI analysis. However, the utility of EHR data for AI depends on its structure and quality. While structured data (e.g., coded diagnoses, lab values) is more easily processed, a vast amount of valuable clinical information resides in unstructured free-text notes, requiring sophisticated Natural Language Processing (NLP) techniques for extraction and analysis.11 Global EHR adoption rates and system maturity vary significantly, impacting the availability and quality of digital data for AI across different regions and health systems.16
Interoperability (FHIR and Beyond): Simply having digitized data in EHRs is insufficient if that data cannot be easily accessed, shared, and combined across different systems and applications. Interoperability—the ability of different IT systems and software applications to communicate, exchange data, and use the information that has been exchanged—is crucial.11 Standards like HL7 FHIR are designed to facilitate this seamless data exchange between EHRs, health information exchanges (HIEs), patient portals, mobile apps, and AI tools.35 FHIR utilizes modern web standards (like RESTful APIs) to make data sharing more flexible, scalable, and easier for developers compared to older standards.35 This is vital for AI, both for aggregating diverse datasets needed for training robust models and for integrating AI-driven insights (e.g., CDS alerts) back into clinicians' primary workflows, often within the EHR.36 While FHIR adoption is growing, particularly in North America where over 75% of EHR systems reportedly incorporate FHIR APIs to some extent 71, its implementation maturity varies globally, representing a key factor in AI readiness.36
Broadband Access & Connectivity: Reliable, high-speed internet connectivity forms the backbone for many modern AI applications in healthcare.3 Many AI platforms are cloud-based, requiring robust connectivity for data transmission and processing. Real-time analysis of data from remote monitoring devices or telehealth platforms depends on stable internet access.73 Furthermore, accessing and working with the large datasets often required for training and validating AI models necessitates significant bandwidth.74 The persistent "digital divide"—disparities in broadband access and affordability between urban and rural areas, or between high-income and low- and middle-income countries (LMICs)—poses a significant barrier to the equitable deployment and use of AI in healthcare.3 While technologies like fibre and Fixed Wireless Access (FWA) are expanding, significant variations in penetration and speed persist across OECD countries and globally.74
Cybersecurity & Data Privacy: Healthcare data is highly sensitive, making robust cybersecurity and data privacy protections paramount for AI adoption.2 AI systems often require access to large volumes of patient information, increasing the potential attack surface and the risks associated with data breaches.53 Maintaining patient trust and ensuring compliance with regulations like HIPAA in the US or GDPR in Europe are critical prerequisites for using patient data to train and deploy AI tools.10 Weak cybersecurity infrastructure or inadequate privacy safeguards can severely hinder AI development and deployment, due to both regulatory non-compliance and the erosion of public and provider trust.6 Global variations in cybersecurity preparedness, as measured by indices like the ITU Global Cybersecurity Index 76, and the strength of data privacy legislation 80 reflect differing levels of readiness to handle the security implications of AI.
Data Governance & Quality: Beyond security and privacy, effective data governance encompasses the policies, standards, and processes for managing the availability, usability, integrity, and quality of data used by AI systems.3 High-quality, accurate, and complete data is essential for training reliable AI models.8 Equally critical is ensuring that training data is representative of the diverse populations on which the AI will be used, to avoid algorithmic bias and promote health equity.7 Adherence to principles like FAIR (Findable, Accessible, Interoperable, Reusable) data is increasingly recognized as important for creating AI-ready datasets.17 Challenges related to data fragmentation across silos, inconsistent data standards, missing data, and inherent biases in historical data represent significant hurdles that require strong governance frameworks to address.11 The quality of a country's regulatory environment, partly reflected in indicators like the World Bank's Worldwide Governance Indicators (WGI) for Regulatory Quality 67, can influence the effectiveness of data governance practices.
4.2 Evidence: Infrastructure as a Determinant of AI Impact
Arguments FOR Infrastructure as Key: A substantial body of evidence underscores the critical role of infrastructure as a determinant of AI's impact in healthcare. Studies and reports consistently identify infrastructural limitations as major barriers. Lack of overall digital maturity and adequate data infrastructure is cited as hampering AI progress, particularly in systems like the NHS and more broadly.32 Difficulties in accessing sufficient volumes of high-quality, diverse, and standardized data are frequently highlighted as impediments to developing, validating, and ensuring the generalizability of AI models.3 This is compounded by poor interoperability between systems, which prevents the seamless data flow necessary for both training AI and integrating it effectively into clinical workflows.8 Connectivity barriers, including lack of access to affordable broadband, pose fundamental challenges, especially in LMICs and rural areas, limiting the feasibility of deploying many AI solutions.3 Furthermore, the lack of necessary technical infrastructure (computing power, storage) and specialized personnel (data scientists, AI experts) within healthcare organizations restricts their capacity to adopt and manage AI technologies. Comparative analyses, such as those contrasting LMICs with HICs 3 or examining geographical variations in AI research focus 2, implicitly suggest that infrastructural differences contribute significantly to the observed variations in AI adoption and application priorities.
Arguments AGAINST Infrastructure as Primary Determinant (or, Other Factors Matter Critically): While essential, infrastructure alone does not guarantee successful AI adoption or impact. Significant challenges persist even in environments with relatively mature digital foundations, indicating that other factors play crucial roles.8 A major hurdle is demonstrating the real-world clinical utility and performance of AI tools beyond controlled research settings.8 Medical providers often remain reluctant to adopt technologies whose benefits in complex, diverse clinical environments are not clearly proven.8 Building and maintaining trust among both clinicians and patients is another critical factor, often hindered by concerns about the "black box" nature of some AI algorithms, potential biases, and ethical implications.6 Regulatory uncertainty and the complexities of navigating approval processes for AI-based medical devices also pose significant barriers.8 Even with technical interoperability, successfully integrating AI into established clinical workflows requires careful consideration of human factors, change management, and potential disruptions to existing practices.8 The lack of an AI-competent healthcare workforce, capable of understanding, utilizing, and critically evaluating AI tools, further limits adoption.7 Finally, the cost of AI solutions and the difficulty in establishing clear funding mechanisms or demonstrating ROI can be prohibitive, independent of the underlying basic infrastructure.8 The effectiveness of AI ultimately relies on successful implementation and adoption by end-users, which is influenced by this broader constellation of factors, not just the availability of technology.11
4.3 Synthesis and Evaluation:
Infrastructure as Necessary but Not Sufficient: The evidence converges on the conclusion that adequate IT and internet infrastructure is a necessary, but not sufficient, condition for realizing the potential of AI in healthcare. Foundational elements like digitized health records (EHRs), robust connectivity, and mechanisms for data exchange (interoperability) are essential prerequisites.35 Without them, the data-intensive nature of most impactful AI applications cannot be supported, creating fundamental barriers, particularly evident in resource-constrained settings or LMICs. However, the numerous instances of slow adoption or implementation failures in settings with relatively advanced infrastructure demonstrate that technology availability alone is not enough.8 The success of AI hinges equally, if not more, on addressing non-infrastructural factors. These include demonstrating clear clinical and economic value 8, ensuring tools are seamlessly integrated into practical workflows 8, building trust through transparency and validation 11, navigating ethical and regulatory complexities 11, aligning incentives 8, and cultivating a workforce capable of using these tools effectively. Therefore, infrastructure acts as a critical enabler or gatekeeper, setting the stage for AI, but achieving meaningful impact requires a holistic approach that addresses the complex interplay of technology, people, processes, and policies.
Interoperability (esp. FHIR) as a Key Accelerator: Within the broader discussion of infrastructure, the capability for seamless data exchange, particularly through modern standards like FHIR, emerges as a crucial accelerator for AI in healthcare.35 The significance extends beyond simply having data in a digital format (i.e., EHR adoption). True value, especially for AI, is unlocked when data becomes liquid – easily and securely movable between systems – and usable – structured in a standardized way that applications can readily consume. AI models often achieve greater accuracy and robustness when trained on diverse data aggregated from multiple sources (e.g., different departments, health systems, or data types like clinical notes, labs, imaging, wearables).1 Furthermore, the practical utility of AI tools, such as CDS systems, depends heavily on their ability to integrate smoothly into existing clinical workflows, which are typically centered around the EHR.8 FHIR, leveraging modern web technologies like APIs and standardized data formats (Resources), is specifically designed to lower the technical barriers to this type of data exchange and application integration compared to older, more rigid standards.35 Research explicitly connects FHIR adoption to enabling better data integration for research and AI/ML applications, improving data quality, and facilitating the deployment of CDS systems.35 Consequently, the maturity of FHIR implementation within a health system or country may serve as a more nuanced and potent indicator of AI readiness than EHR penetration rates alone, as it directly addresses the critical needs for both data aggregation (for model development) and tool integration (for practical application).
5. Healthcare Payment Models: Shaping AI Adoption and Incentives
Introduction: Healthcare payment models – the mechanisms by which providers are compensated for the services they render – establish the financial landscape and incentive structures within which healthcare organizations operate. These structures profoundly influence decisions regarding the adoption of new technologies, including AI.9 Whether a health system primarily operates under a traditional Fee-for-Service (FFS) model, has transitioned towards Value-Based Care (VBC) arrangements (such as Accountable Care Organizations (ACOs) or bundled payments), or utilizes Capitation models significantly shapes the perceived value and economic feasibility of different AI applications.
5.1 How Payment Models Influence AI Adoption:
Fee-for-Service (FFS): The traditional FFS model reimburses providers for each distinct service or procedure performed.85 This inherently incentivizes volume of care. Within an FFS environment, AI adoption is more likely to be favored if the technology directly increases the volume of billable services, enhances the efficiency of delivering those services (allowing more to be done in the same timeframe), or qualifies as a separately reimbursable service itself.21 For example, an AI tool that improves the throughput of diagnostic imaging reads or surgical procedures might align well with FFS incentives. Similarly, AI tools that receive specific reimbursement codes, like the IDx-DR system for diabetic retinopathy screening, find a clearer path to adoption in FFS settings. Conversely, FFS models may create disincentives for adopting AI applications focused on prevention, reducing unnecessary tests or procedures, or improving long-term health outcomes if these actions lead to a reduction in billable services.
Value-Based Care (VBC): VBC models represent a shift away from volume towards rewarding value, defined as achieving better patient outcomes at lower costs.65 Payment in VBC arrangements is often linked to quality metrics, patient satisfaction, cost efficiency, and overall population health management.9 This structure creates fundamentally different incentives for technology adoption. AI tools that enhance diagnostic accuracy (reducing misdiagnosis-related costs and improving outcomes), predict patient risk (allowing for early intervention), improve care coordination, optimize treatment plans based on effectiveness, manage population health proactively, and ultimately reduce hospitalizations or long-term costs are highly aligned with VBC goals.9 AI is also valuable for the data analytics required to track, measure, and report on the quality and cost metrics central to VBC contracts.10 The explicit goal of major payers like CMS to move towards VBC 91 and support from organizations like the AMA 75 signal a policy environment increasingly conducive to AI applications that demonstrate value in this context.
Capitation: Under capitated models, providers receive a fixed, predetermined payment per patient for a defined period, regardless of the number or type of services provided.85 This places the financial risk squarely on the provider, creating strong incentives to manage costs effectively and keep patients healthy.85 AI applications that enhance operational efficiency, promote preventive care, enable effective chronic disease management to avoid acute episodes, and facilitate conservative, evidence-based treatment pathways align well with the financial incentives of capitation.85 However, a potential downside is that an excessive focus on cost containment could lead to underutilization of necessary services or incentives to avoid enrolling sicker, more complex patients if AI is used primarily for cost reduction without adequate quality safeguards.85
Return on Investment (ROI) and Funding: Regardless of the specific payment model, securing funding for AI adoption requires a convincing demonstration of ROI.9 However, what constitutes "value" or a positive ROI differs significantly depending on the payment structure. In FFS, ROI might be measured in increased billings or faster throughput of reimbursed procedures. In VBC or capitation, ROI is more likely tied to reduced hospitalizations, improved quality scores leading to bonuses, or long-term cost avoidance.10 The complexity of healthcare payment systems, often involving multiple payers with different rules, combined with the financial pressures faced by many health systems, makes demonstrating this ROI and securing stable funding a significant challenge for AI adoption.9 The lack of clear, standardized reimbursement pathways specifically for AI tools further complicates the financial justification.87
5.2 Evidence: Payment Models as a Determinant of AI Impact
Arguments FOR Payment Models as Key: Evidence strongly suggests that payment models act as a powerful determinant shaping the adoption and impact of AI in healthcare. Health systems explicitly prioritize different types of AI tools based on how they are compensated; for example, revenue-generating departments may invest differently than systems focused on population health under VBC.9 The shift towards VBC is frequently cited as a major catalyst for adopting AI tools that focus on outcome measurement, predictive analytics for risk stratification and prevention, care coordination, and demonstrating quality improvements – capabilities less directly rewarded under FFS.10 Conversely, the misalignment between simple "pay-per-use" reimbursement approaches for AI and the broader goals of VBC highlights how payment structures can hinder the adoption of AI for holistic value creation.87 The fundamental principle that financial incentives drive provider behavior is well-established in healthcare 86, making payment reform a critical lever for influencing technology adoption, including AI.52
Arguments AGAINST Payment Models as Primary Determinant (or, Other Factors Matter Critically): While payment models create the incentive landscape, they do not operate in isolation, and other factors can override or significantly moderate their influence. Even where payment models theoretically favor AI (e.g., VBC), adoption can be sluggish or fail due to persistent non-financial barriers.64 These include the fundamental challenges of building clinician and patient trust in AI technologies 12, addressing concerns about algorithmic bias and equity 7, navigating complex regulatory approvals 87, and overcoming practical difficulties in integrating AI into complex clinical workflows.48 The lack of transparency and explainability in some AI models can create resistance regardless of potential financial benefits.7 Furthermore, organizational factors like leadership commitment, the availability of skilled personnel, and the capacity for change management are crucial for successful implementation, irrespective of the payment environment.26 Non-financial benefits, such as improved quality of care, enhanced patient experience, or reduced clinician burnout, can also be powerful drivers for AI adoption, sometimes even in the absence of direct financial incentives under certain payment models.21
5.3 Synthesis and Evaluation:
Payment Models Fundamentally Shape the "Value Proposition" of AI: The analysis strongly indicates that healthcare payment models play a fundamental role in defining the "value proposition" of AI technologies within a given health system. They act as a powerful filter, determining which AI capabilities are perceived as economically viable and strategically important, thereby shaping investment priorities and adoption patterns.9 In systems dominated by FFS, value is often equated with increased service volume or direct reimbursement for the AI tool itself, favoring applications that enhance throughput or fit into existing billing codes. In contrast, VBC models redefine value around improved patient outcomes, cost-effectiveness, and population health management. This shift makes AI applications focused on predictive analytics, risk stratification, care coordination, quality improvement, and long-term cost reduction significantly more attractive and justifiable from a financial perspective.10 Similarly, capitation models prioritize cost control and prevention, aligning incentives with AI tools that enhance operational efficiency and support proactive health management.85 Consequently, the prevailing payment structure within a health system or country heavily influences the types of AI solutions that are likely to be developed, adopted, and scaled.
The Transition to VBC is a Catalyst, but Implementation Complexity is a Drag: While the global trend towards VBC theoretically creates a more fertile ground for impactful AI adoption, the practical realities and complexities of implementing VBC itself can act as a significant drag on this potential synergy.64 VBC's emphasis on outcomes, quality, and cost aligns naturally with the capabilities of AI in data analysis, prediction, personalization, and efficiency improvement.10 This alignment provides a strong rationale for investing in AI tools that can help providers succeed under these new payment arrangements. However, VBC models often introduce substantial complexity for providers, involving intricate performance metrics, complex patient attribution rules, demanding data reporting requirements, and significant financial risk.64 Healthcare organizations may find themselves dedicating considerable resources and attention simply to navigating the administrative and analytical burdens of participating in VBC programs. This can leave limited bandwidth, resources, or organizational capacity to simultaneously undertake the challenging task of selecting, integrating, and validating complex AI technologies.64 Furthermore, the fragmentation of VBC initiatives often seen within health plans can create conflicting signals and add layers of inefficiency.64 Thus, while AI holds the potential to help manage VBC complexity and achieve its goals 64, the initial burden of VBC implementation might paradoxically slow down the adoption of the very AI tools that could facilitate its success. This suggests a need for strategies that simplify VBC models while concurrently promoting the adoption of supportive AI technologies.
6. Evaluating the Hypothesis: Does AI Impact Vary with Infrastructure and Payment Models?
Restatement of Hypothesis: The central hypothesis under examination is that the impact of AI across key healthcare dimensions—quality of care, cost of care, provider and patient experience, and population health outcomes—significantly varies depending on the synergistic influence of a region's or system's IT/internet infrastructure and its prevailing healthcare payment models.
Synthesis of Evidence:
Evidence Supporting Variation: The evidence gathered strongly supports the hypothesis that AI's realized impact is not uniform but is significantly modulated by infrastructural readiness and financial incentives. Comparative analyses reveal disparities in AI adoption and focus linked to infrastructure maturity. For instance, LMICs face fundamental barriers due to limited ICT infrastructure and connectivity compared to HICs, although they may possess advantages in leapfrogging legacy systems.3 Within developed systems like the NHS, inadequate digital maturity and data access challenges hinder AI progress.59 Geographical variations in AI research priorities also suggest underlying differences in infrastructural capacity and focus.2 Similarly, payment models demonstrably shape AI priorities; health systems operating under FFS value AI differently than those under VBC or capitation, leading to the selection of different types of AI tools.9 The move towards VBC is consistently identified as a catalyst for adopting AI focused on improving outcomes and efficiency, areas less incentivized by FFS.10 The interaction between these factors is also evident: advanced, interoperable infrastructure (like FHIR-enabled systems 36) is necessary to generate and analyze the data required for success in VBC 64, while VBC provides the financial rationale for investing in such infrastructure and the AI tools it supports.10 Systems lacking in either robust infrastructure or aligned incentives face significant limitations in leveraging AI effectively.
Evidence Against Sole Determinism / Nuances: While infrastructure and payment models are critical, the evidence also clearly indicates they are not the sole determinants of AI's success or failure.7 Numerous other factors exert significant influence, often irrespective of the infrastructural or financial context. These include the establishment of clear governance frameworks and regulatory pathways 8, the availability of a skilled workforce capable of developing and utilizing AI 3, the practicalities of integrating AI into complex clinical workflows 8, the crucial elements of clinician and patient trust 11, and addressing ethical concerns, particularly regarding data privacy and algorithmic bias.7 The perceived clinical need and demonstrated real-world value of an AI application can also drive adoption even when financial incentives are ambiguous.8 Therefore, a purely techno-economic determinism is insufficient to explain the observed patterns of AI impact.
Assessment of the Hypothesis: The evidence strongly supports the core hypothesis. While the potential applications of AI in healthcare might appear universal, the realized impact across the dimensions of quality, cost, experience, and population health is demonstrably and significantly shaped by the interplay between digital infrastructure and payment models. Infrastructure maturity acts as a foundational enabler, determining the technical feasibility of deploying AI tools and the availability of data to power them. Payment models provide the crucial incentive structure, defining what constitutes "value" and influencing which AI applications offer a viable return on investment. Systems characterized by both mature, interoperable digital infrastructure and payment models aligned with value creation (such as well-implemented VBC) are best positioned to harness AI for transformative improvements. Conversely, systems burdened by inadequate infrastructure, fragmented data ecosystems, or payment models that primarily incentivize volume (like traditional FFS) will likely experience slower, more limited, or narrowly focused AI adoption, restricting its overall impact on healthcare transformation. The combination of these two factors creates a clear gradient of AI readiness and potential impact across different healthcare systems globally.
The Interdependence Creates a "Readiness Spectrum": It is crucial to recognize that IT infrastructure and payment models are not merely independent variables influencing AI adoption; they are often deeply intertwined and exert reciprocal influence, creating a spectrum of AI readiness across different health systems. Significant investments are required to build and maintain advanced digital infrastructure, including interoperable EHRs, robust data analytics platforms, and secure cloud environments.8 Value-based payment models, with their focus on long-term outcomes, population health, and cost efficiency, can provide the necessary business case and financial justification for undertaking these substantial infrastructure investments, which might be harder to rationalize under a purely FFS system focused on short-term transactional revenue.10 Conversely, a mature and interoperable digital infrastructure is essential for collecting, aggregating, and analyzing the complex patient and population data needed to successfully manage risk, measure quality, and demonstrate value under VBC arrangements.36 Systems lagging in both infrastructure development and payment reform face a compounded challenge, lacking both the technical means and the financial incentives to effectively leverage AI. This interdependence implies that policy initiatives aiming to accelerate the beneficial impact of AI in healthcare are likely to be most effective when they address infrastructure modernization and payment model reform concurrently, recognizing their synergistic relationship in shaping a system's overall AI readiness.
7. Key Discerning Factors Shaping Global AI Impact in Healthcare
Based on the analysis of how infrastructure, payment models, and other critical elements influence AI's role in healthcare, five key factors emerge as the most significant differentiators of potential or realized AI impact globally. These factors synthesize the core prerequisites and enablers discussed throughout the report.
Table 1: Top 5 Discerning Factors for AI Impact in Healthcare
Factor
Description
Supporting Evidence
Rationale
1. Digital Infrastructure Maturity
Encompasses the availability, quality, and penetration of foundational digital technologies within a country's healthcare ecosystem. This includes broadband and mobile connectivity (e.g., 4G/5G), adoption rates and sophistication of Electronic Health Records (EHRs), utilization of cloud computing, and the overall technological capacity to support data-intensive applications.
2-73-94-96,,,,
This factor represents the fundamental technical capability required to deploy, run, and access AI tools and the data they rely on. Without adequate connectivity and digitized data sources, most advanced AI applications are simply not feasible. Variations in maturity create significant disparities in AI readiness.
2. Data Governance, Interoperability & Privacy Frameworks
Includes the existence, clarity, and enforcement of comprehensive data privacy laws (e.g., GDPR-like regulations), established data governance policies within health systems, widespread adoption of technical interoperability standards (especially modern ones like FHIR), and the overall legal and regulatory environment governing the ethical access, sharing, and use of health data for AI development and deployment.
3-7-67-84,
This factor determines the ability to legally, ethically, and efficiently access and utilize the high-quality, diverse data essential for training and validating effective and unbiased AI models. It also governs the secure integration of AI into workflows and builds public trust. Weaknesses here create major bottlenecks and risks.
3. AI Talent Pool & Digital Skills
Refers to the availability and concentration of human capital with the necessary expertise to drive AI innovation and adoption in healthcare. This includes data scientists, machine learning engineers, AI researchers, software developers, as well as a digitally literate clinical workforce capable of using and critically evaluating AI tools. It also encompasses the strength of the education system in producing this talent and initiatives for upskilling existing professionals.
3-95-98-101,
AI development and implementation are human-intensive activities. A shortage of skilled personnel is a frequently cited barrier to AI progress globally. Countries with strong talent pipelines and digital skills across the workforce are better positioned to innovate and adopt AI effectively.
4. Investment & Funding Environment
Covers the overall level of financial commitment to AI in healthcare from both public and private sources. This includes government funding for AI research and development (R&D), national AI strategies with dedicated budgets, venture capital (VC) investment flowing into health AI startups, and the general economic capacity and willingness to fund large-scale AI implementation projects within health systems.
3,,
AI development and deployment require significant financial resources. Access to capital fuels innovation, supports startups, enables infrastructure upgrades, and funds implementation projects. Variations in investment levels directly impact the pace and scale of AI adoption.
5. Payment System Alignment & VBC Adoption
The extent to which a country's dominant healthcare payment models create financial incentives that align with the potential value generated by AI (e.g., improving quality, efficiency, long-term outcomes). This includes the prevalence of Value-Based Care (VBC) models versus traditional Fee-for-Service (FFS), and the regulatory clarity regarding reimbursement for AI-enabled services or AI's contribution to achieving value targets.
9,,,,,,,,,
Payment models fundamentally shape the economic rationale for adopting AI. Misaligned incentives (e.g., FFS rewarding volume over value) can stifle the adoption of beneficial AI, while aligned models (like VBC) can catalyze investment in AI that demonstrably improves outcomes and efficiency. This factor determines the financial sustainability of AI integration.
These five factors represent distinct but interconnected domains that collectively shape a country's capacity to successfully leverage AI for healthcare transformation. Strengths or weaknesses in any one area can significantly impact overall progress.
8. Global Readiness Snapshot: Top 10 Country Rankings
Introduction: To provide a comparative perspective on global readiness for AI in healthcare, this section presents Top 10 country rankings for each of the five discerning factors identified previously. These rankings are derived from synthesizing data from relevant and reputable global indices and comparative reports. It is important to acknowledge the limitations inherent in such rankings: data availability varies, index methodologies differ, underlying data may have time lags, and rankings provide a snapshot rather than a complete picture of a complex reality. However, they offer valuable benchmarks for understanding relative strengths and weaknesses across nations.
8.1 Factor 1: Digital Infrastructure Maturity Rankings:
This factor assesses the foundational technological capacity. Key indices considered include the ITU ICT Development Index (IDI) 92, the Network Readiness Index (NRI) 107, the IMD World Digital Competitiveness Ranking (Technology factor) 96, the UN E-Government Development Index (EGDI - Telecommunication Infrastructure Index component) 93, and OECD broadband data.73 Countries consistently ranking high across these indices demonstrate superior connectivity, technology adoption, and digital infrastructure relevant to healthcare AI.
Top 10 Countries (Digital Infrastructure Maturity - Synthesis):
Singapore
South Korea
Denmark
United States
Sweden
Finland
Netherlands
Switzerland
United Arab Emirates
Hong Kong SAR
Justification: These countries consistently appear in the top tiers of the IDI, NRI, EGDI (TII), and IMD Digital Competitiveness rankings, reflecting high levels of broadband and mobile penetration, advanced ICT infrastructure, strong 4G/5G coverage, and high levels of technology adoption critical for AI deployment. Singapore, South Korea, and several Nordic/European nations frequently lead in these metrics.92 The US also performs strongly, particularly in network readiness and overall ICT development.92
8.2 Factor 2: Data Governance, Interoperability & Privacy Frameworks Rankings:
This factor evaluates the legal, regulatory, and technical environment for accessing and using health data ethically and efficiently. Sources include assessments of data privacy law coverage and strength 80, the World Bank Worldwide Governance Indicators (WGI) focusing on Regulatory Quality and Rule of Law 67, the ITU Global Cybersecurity Index (GCI - Legal Measures pillar) 76, the NRI Governance pillar 108, and qualitative assessments of interoperability standard adoption (e.g., FHIR progress 71).
Top 10 Countries (Data Governance, Interoperability & Privacy - Synthesis):
Estonia
Germany
Denmark
Finland
Singapore
Netherlands
United Kingdom
Sweden
Norway
France
Justification: European countries benefit from the comprehensive GDPR framework, reflected in strong data privacy assessments and often high WGI Regulatory Quality scores.80 Estonia is a recognized leader in digital governance and secure data exchange.92 Singapore also scores highly on government effectiveness and regulatory aspects supporting digital initiatives.92 These countries generally exhibit strong legal frameworks (reflected in GCI Tier 1 status for many 78) and efforts towards health data interoperability.
8.3 Factor 3: AI Talent Pool & Digital Skills Rankings:
This factor assesses the availability of human capital necessary for AI development and adoption in healthcare. Key indices include the Global Talent Competitiveness Index (GTCI) 98, the IMD World Talent Ranking 98, and the Tortoise Global AI Index (Talent sub-pillar).102 Indicators related to education quality, availability of scientists and engineers, digital skills in the workforce, and ability to attract international talent are relevant.
Top 10 Countries (AI Talent Pool & Digital Skills - Synthesis):
Switzerland
United States
Singapore
Denmark
Sweden
Finland
Netherlands
Luxembourg
Norway
Germany
Justification: Switzerland consistently tops talent rankings like GTCI and IMD World Talent Ranking due to its high quality of life, excellent education system, and ability to attract and retain talent.98 The US leads in AI research and has a large pool of specialized talent, reflected in the Tortoise AI Index and GTCI.102 Singapore also performs exceptionally well in attracting global talent and developing skills.102 Nordic countries and the Netherlands consistently rank highly on education, skills readiness, and appeal factors.98
8.4 Factor 4: Investment & Funding Environment Rankings:
This factor measures the financial resources available for AI R&D and adoption in healthcare. Sources include the Tortoise Global AI Index (Investment and Commercial pillars) 102, data on venture capital (VC) funding directed towards health AI startups 16, information on government investment in national AI strategies 104, and general R&D expenditure data from sources like the OECD.
Top 10 Countries (Investment & Funding Environment - Synthesis):
United States
China
United Kingdom
Singapore
Israel
Canada
Germany
France
South Korea
India
Justification: The US dominates in VC funding for AI and has a highly developed commercial AI ecosystem, leading the Tortoise AI Index investment and commercial pillars.16 China shows massive state-backed investment and a rapidly growing commercial AI sector.16 The UK, Israel, Canada, and Germany have strong startup ecosystems and significant AI investment.102 Singapore benefits from strong government support and a strategic focus on AI.102 India is emerging as a significant player with a large market and growing investment.102
8.5 Factor 5: Payment System Alignment & VBC Adoption Rankings:
This factor assesses the extent to which healthcare financing incentivizes the use of AI for value. Direct comparative indices are scarce. Ranking relies on synthesizing information from Commonwealth Fund reports on health system performance, efficiency, and equity (which often correlate with VBC maturity) 91, OECD data on spending efficiency 69, and qualitative assessments of national policies promoting VBC and clarifying AI reimbursement.86
Top 10 Countries (Payment System Alignment & VBC Adoption - Qualitative Synthesis):
Netherlands
Australia
United Kingdom
Germany
Switzerland
Norway (based on 2021 Mirror Mirror data)
Sweden
New Zealand
France
Canada
Justification: Countries like the Netherlands, Australia, and the UK consistently rank high in Commonwealth Fund reports for overall performance, access, and efficiency, often employing universal coverage systems with established mechanisms for quality improvement and cost control, elements conducive to VBC principles.117 Germany and Switzerland have well-regulated universal systems balancing private delivery with strong oversight.120 Nordic countries generally perform well on efficiency and outcomes.119 While the US has significant VBC initiatives 91, its overall system performance, particularly on access, equity, and outcomes, ranks last among peers, indicating challenges in achieving widespread value alignment despite policy efforts.117
Table 2: Consolidated Top 10 Country Rankings Across Factors
Rank
Digital Infrastructure Maturity
Data Governance, Interoperability & Privacy
AI Talent Pool & Digital Skills
Investment & Funding Environment
Payment System Alignment & VBC Adoption
1
Singapore
Estonia
Switzerland
United States
Netherlands
2
South Korea
Germany
United States
China
Australia
3
Denmark
Denmark
Singapore
United Kingdom
United Kingdom
4
United States
Finland
Denmark
Singapore
Germany
5
Sweden
Singapore
Sweden
Israel
Switzerland
6
Finland
Netherlands
Finland
Canada
Norway*
7
Netherlands
United Kingdom
Netherlands
Germany
Sweden
8
Switzerland
Sweden
Luxembourg
France
New Zealand
9
United Arab Emirates
Norway
Norway
South Korea
France
10
Hong Kong SAR
France
Germany
India
Canada
Note: Norway's ranking in the Payment System Alignment category is inferred from its top performance in the 2021 Commonwealth Fund report, as it was not included in the 2024 analysis. This table highlights countries like Singapore, the US, and several Northern European nations that demonstrate strengths across multiple dimensions critical for AI success in healthcare. It also reveals that leadership in one area (e.g., Investment in the US and China) does not guarantee top performance in others (e.g., Payment System Alignment or Data Governance).
9. Conclusion and Strategic Recommendations
Summary of Findings: This report confirms that the impact of Artificial Intelligence in healthcare is not uniform globally. The central hypothesis—that the effectiveness and adoption of AI across quality, cost, experience, and population health dimensions are significantly modulated by IT/internet infrastructure and healthcare payment models—is strongly supported by the evidence. Mature digital infrastructure provides the necessary foundation for data-intensive AI applications, while aligned payment models, particularly those emphasizing value-based care, create the crucial incentives for their adoption and scaling. However, these two factors, while critical, are necessary but not sufficient. Realizing AI's potential also hinges on robust data governance, clear regulatory frameworks, a skilled workforce, successful workflow integration, and the cultivation of trust among clinicians and patients. The interplay of these technological, financial, organizational, ethical, and human factors creates a complex landscape where AI readiness varies considerably across nations, as reflected in the global rankings across key discerning factors.
Strategic Recommendations: Harnessing the transformative potential of AI in healthcare requires concerted and coordinated action from various stakeholders.
For Policymakers:
Develop Integrated Strategies: Create comprehensive national AI-in-health strategies that simultaneously address infrastructure development, payment model reform, data governance, ethical guidelines, and workforce training needs. Avoid siloed approaches.3
Invest in Foundational Infrastructure: Prioritize public and private investment in universal broadband access, promote the adoption of mature, interoperable EHR systems, and mandate or incentivize the use of modern interoperability standards like FHIR to ensure data liquidity.3
Accelerate Value-Based Payment Reform: Actively promote and refine value-based payment models that reward improved health outcomes and efficiency, creating clear financial incentives for adopting beneficial AI technologies. Work towards clarifying reimbursement pathways for AI-driven services and analyses within these models.64
Establish Clear Governance and Regulation: Develop clear, agile, and harmonized regulatory frameworks for the safe, effective, and ethical development and deployment of AI in healthcare. This includes standards for validation, bias mitigation, transparency, and liability. Foster public trust through open dialogue, engagement, and robust data privacy and security enforcement.7
Cultivate AI Talent and Digital Literacy: Invest in educational programs to build a pipeline of AI specialists and data scientists. Implement initiatives to enhance the digital literacy of the existing healthcare workforce, enabling them to effectively use and critically appraise AI tools.3
For Health Systems & Providers:
Establish Internal AI Governance: Create dedicated committees or roles (e.g., Chief AI Officer) to oversee AI strategy, procurement, implementation, and monitoring, ensuring alignment with organizational goals and ethical principles.26
Prioritize Strategically: Select AI applications that address clear clinical or operational needs and offer demonstrable value aligned with the prevailing payment models and organizational priorities. Consider starting with lower-risk, high-impact administrative applications to build capacity and trust.9
Focus on Workflow Integration and User Buy-in: Ensure AI tools are seamlessly integrated into existing clinical workflows, minimizing disruption and maximizing usability. Engage clinicians early and continuously in the selection and implementation process to foster adoption and trust.8
Invest in Data Readiness: Assess and improve internal data quality, standardization, and infrastructure to support AI initiatives. Pursue strategic partnerships with technology vendors to leverage external expertise while ensuring solutions meet specific needs.50
For AI Developers:
Design for Real-World Needs: Develop AI solutions that address genuine clinical or administrative pain points and are designed for practical integration into complex healthcare environments.8
Prioritize Trustworthiness: Emphasize transparency, explainability, and rigorous bias detection and mitigation in algorithm design and validation. Proactively address ethical considerations.7
Generate Robust Evidence: Invest in high-quality clinical trials and real-world evidence generation to demonstrate the safety, efficacy, and economic value of AI tools across diverse patient populations and clinical settings.8
Ensure Compliance: Design solutions that meet stringent regulatory requirements (e.g., FDA, CE marking) and comply with data privacy laws (e.g., HIPAA, GDPR) in target markets.34
Future Outlook: The integration of AI into healthcare is an ongoing journey, not a destination. Technologies will continue to evolve rapidly, particularly in areas like generative AI and multimodal models.50 Successfully navigating this evolution requires sustained commitment from all stakeholders. Continuous collaboration between policymakers, healthcare providers, researchers, developers, and patients will be essential. Ethical vigilance must remain paramount, ensuring that AI is developed and deployed in ways that promote equity, protect privacy, and maintain human control over critical decisions.61 Adaptive strategies, ongoing evaluation of real-world impact, and a willingness to adjust course based on evidence will be crucial for harnessing the full potential of AI to improve health and well-being globally, ensuring that its benefits are shared equitably and contribute to building more resilient and effective healthcare systems for the future.2
Works cited
A Review on Revolutionizing Healthcare Technologies with AI and ML Applications in Pharmaceutical Sciences - MDPI, accessed April 12, 2025, https://www.mdpi.com/2813-2998/4/1/9
Exploring the Impact of Artificial Intelligence on Healthcare ... - MDPI, accessed April 12, 2025, https://www.mdpi.com/2076-3417/14/22/10144
www.broadbandcommission.org, accessed April 12, 2025, https://www.broadbandcommission.org/Documents/working-groups/AIinHealth_Report.pdf
Exploring Artificial Intelligence in Healthcare: A Precise Review | Journal of Bio-X Research, accessed April 12, 2025, https://mednexus.org/doi/full/10.34133/jbioxresearch.0025
AI in the workplace: A report for 2025 - McKinsey, accessed April 12, 2025, https://www.mckinsey.com/capabilities/mckinsey-digital/our-insights/superagency-in-the-workplace-empowering-people-to-unlock-ais-full-potential-at-work
Trending Topics: Artificial Intelligence (AI) in Healthcare - Veradigm, accessed April 12, 2025, https://veradigm.com/artificial-intelligence-healthcare/
Artificial Intelligence In Health And Health Care: Priorities For Action - Health Affairs, accessed April 12, 2025, https://www.healthaffairs.org/doi/10.1377/hlthaff.2024.01003
www.gao.gov, accessed April 12, 2025, https://www.gao.gov/assets/gao-22-104629.pdf
Moving Ahead of the Pack: Understanding Health System Priorities ..., accessed April 12, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10508856/
With AI, keep patient satisfaction top of mind, says health IT investor ..., accessed April 12, 2025, https://www.healthcareitnews.com/news/ai-keep-patient-satisfaction-top-mind-says-health-it-investor
Barriers to and Facilitators of Artificial ... - JMIR Human Factors, accessed April 12, 2025, https://humanfactors.jmir.org/2024/1/e48633
Physicians and AI in healthcare: insights from a mixed-methods study in Poland on adoption and challenges - Frontiers, accessed April 12, 2025, https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1556921/full
Artificial Intelligence (AI) Applications in Drug Discovery and Drug Delivery: Revolutionizing Personalized Medicine - MDPI, accessed April 12, 2025, https://www.mdpi.com/1999-4923/16/10/1328
Artificial Intelligence (AI) in Health Care - CRS Reports - Congress.gov, accessed April 12, 2025, https://crsreports.congress.gov/product/pdf/R/R48319
AI & RPA in Healthcare- Trends, Use Cases & Benefits, accessed April 12, 2025, https://automationedge.com/home-health-care-automation/blogs/ai-and-rpa-in-healthcare/
The Future of Healthcare: How China's medical industry is adopting AI - CKGSB Knowledge, accessed April 12, 2025, https://english.ckgsb.edu.cn/knowledge/article/the-future-of-healthcare-how-chinas-medical-industry-is-adopting-ai/
NIH STRATEGIC PLAN FOR DATA SCIENCE 2023-2028, accessed April 12, 2025, https://datascience.nih.gov/sites/default/files/NIH-STRATEGIC-PLAN-FOR-DATA-SCIENCE-2023-2028-final-draft.pdf
How AI is improving diagnostics and health outcomes - The World Economic Forum, accessed April 12, 2025, https://www.weforum.org/stories/2024/09/ai-diagnostics-health-outcomes/
AI for IMPACTS Framework for Evaluating the Long-Term Real-World Impacts of AI-Powered Clinician Tools: Systematic Review and Narrative Synthesis - PMC, accessed April 12, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11840377/
A Systematic Review of the Barriers to the Implementation of Artificial Intelligence in Healthcare - PMC - PubMed Central, accessed April 12, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10623210/
What happens when AI comes to healthcare - CEPR, accessed April 12, 2025, https://cepr.org/voxeu/columns/what-happens-when-ai-comes-healthcare
6 ways AI is transforming healthcare - The World Economic Forum, accessed April 12, 2025, https://www.weforum.org/stories/2025/03/ai-transforming-global-health/
AI for Healthcare: How AI Will Transform Patient Care and Health Management in 2025, accessed April 12, 2025, https://www.vonage.com/resources/articles/ai-for-healthcare/
How AI Enhances Diagnostic Accuracy in Clinical Decision Support - Treatment.com, accessed April 12, 2025, https://www.treatment.com/blogs/how-ai-enhances-diagnostic-accuracy-in-clinical-decision-support/
Artificial intelligence in diagnosing medical conditions and impact on healthcare - MGMA, accessed April 12, 2025, https://www.mgma.com/articles/artificial-intelligence-in-diagnosing-medical-conditions-and-impact-on-healthcare
An integrative review on the acceptance of artificial intelligence among healthcare professionals in hospitals - PMC, accessed April 12, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10257646/
Five AI Innovations That Will Redefine Healthcare In 2025 - Forbes, accessed April 12, 2025, https://www.forbes.com/councils/forbestechcouncil/2025/02/28/five-ai-innovations-that-will-redefine-healthcare-in-2025/
AI and public health – a major opportunity | Healthcare IT News, accessed April 12, 2025, https://www.healthcareitnews.com/news/ai-and-public-health-major-opportunity
Can AI Improve Medical Diagnostic Accuracy? | Stanford HAI, accessed April 12, 2025, https://hai.stanford.edu/news/can-ai-improve-medical-diagnostic-accuracy
Advancing Healthcare AI Governance: A Comprehensive Maturity Model Based on Systematic Review | medRxiv, accessed April 12, 2025, https://www.medrxiv.org/content/10.1101/2024.12.30.24319785v1.full-text
How health AI can be a physician's “co-pilot” to improve care, accessed April 12, 2025, https://www.ama-assn.org/practice-management/digital/how-health-ai-can-be-physician-s-co-pilot-improve-care
AI in the Health Sector: Systematic Review of Key Skills for Future Health Professionals, accessed April 12, 2025, https://mededu.jmir.org/2025/1/e58161
How Does AI Reduce Costs in Healthcare: Facts from 7 Startups - Glorium Technologies, accessed April 12, 2025, https://gloriumtech.com/ai-reducing-healthcare-costs/
Artificial Intelligence - NIH Office of Science Policy, accessed April 12, 2025, https://osp.od.nih.gov/policies/artificial-intelligence/
FHIR Adoption: Overcoming Challenges and Benefits, accessed April 12, 2025, https://healthconnect.mindbowser.com/fhir-adoption-in-healthcare/
How the FHIR Data Standard Advances Patient-Centered Care, Healthcare AI Innovation, accessed April 12, 2025, https://cloudwars.com/innovation-leadership/how-fhir-healthcare-data-standard-supports-patient-centered-care-ai-innovation/
How Automation is Transforming Healthcare Administration - Topflight Apps, accessed April 12, 2025, https://topflightapps.com/ideas/automation-healthcare-administration/
Innovative AI in Healthcare: Boosting Efficiency and Reducing Costs - Number Analytics, accessed April 12, 2025, https://www.numberanalytics.com/blog/ai-healthcare-efficiency-cost-reduction
The Future of AI in Healthcare – 2025 | SS&C Blue Prism, accessed April 12, 2025, https://www.blueprism.com/resources/blog/the-future-of-ai-in-healthcare/
The Impact of AI on Process Automation and Resource Savings in Healthcare - Arkangel AI, accessed April 12, 2025, https://www.arkangel.ai/blog-ai/the-impact-of-ai-on-process-automation-and-resource-savings-in-healthcare
The Role of AI in Patient Care | Levo Health, accessed April 12, 2025, https://levohealth.com/the-role-of-ai-in-patient-care/
Physicians' greatest use for AI? Cutting administrative burdens, accessed April 12, 2025, https://www.ama-assn.org/practice-management/digital/physicians-greatest-use-ai-cutting-administrative-burdens
HIMSSCast - Buzzsprout, accessed April 12, 2025, https://feeds.buzzsprout.com/728309.rss
Analysis: AI scribes save physicians time, improve patient interactions and work satisfaction, accessed April 12, 2025, https://permanente.org/analysis-ai-scribes-save-physicians-time-improve-patient-interactions-and-work-satisfaction/
Leveraging AI To Improve Public Health | StateTech Magazine, accessed April 12, 2025, https://statetechmagazine.com/article/2025/02/leveraging-ai-improve-public-health
scholar.harvard.edu, accessed April 12, 2025, https://scholar.harvard.edu/sites/scholar.harvard.edu/files/cutler/files/2024_nber_economicsofai_chapter_2.pdf
AI & Predictive Analytics for Population Health Management - Innovaccer, accessed April 12, 2025, https://innovaccer.com/resources/blogs/the-role-of-ai-predictive-analytics-population-health-management
Adoption of Artificial Intelligence in Healthcare Delivery Systems: Early Applications and Impacts - Peterson Health Technology Institute, accessed April 12, 2025, https://phti.org/wp-content/uploads/sites/3/2025/03/PHTI-Adoption-of-AI-in-Healthcare-Delivery-Systems-Early-Applications-Impacts.pdf
Enhancing Physician Satisfaction and Patient Safety Through an Artificial Intelligence–Driven Scheduling System in Anesthesiology | Ochsner Journal, accessed April 12, 2025, https://www.ochsnerjournal.org/content/25/1/44
Generative AI in healthcare: Current trends and future outlook | McKinsey, accessed April 12, 2025, https://www.mckinsey.com/industries/healthcare/our-insights/generative-ai-in-healthcare-current-trends-and-future-outlook
2025 global health care outlook | Deloitte Insights, accessed April 12, 2025, https://www2.deloitte.com/us/en/insights/industry/health-care/life-sciences-and-health-care-industry-outlooks/2025-global-health-care-executive-outlook.html
AI, Healthcare Innovation, and the Path to Better Outcomes with Dr ..., accessed April 12, 2025, https://salessparx.com/sparxcast-unleashed-podcast/mitch-morris
AI Healthcare Innovation Governance | Protiviti United States, accessed April 12, 2025, http://www.uk.uat-v2.protiviti.com/us-en/whitepaper/ai-healthcare-innovation-governance
Harnessing AI to reshape consumer experiences in healthcare - McKinsey, accessed April 12, 2025, https://www.mckinsey.com/industries/healthcare/our-insights/harnessing-ai-to-reshape-consumer-experiences-in-healthcare
How AI-Powered Solutions Enhance Patient Experience - Thoughtful AI, accessed April 12, 2025, https://www.thoughtful.ai/blog/how-ai-powered-solutions-enhance-patient-experience
Personalized AI-Powered Solutions for Better Patient Adherence - Pharmaceutical Executive, accessed April 12, 2025, https://www.pharmexec.com/view/personalized-ai-powered-solutions-better-patient-adherence
Transforming Patient Care: The Role of AI-Powered Assistants - MedCity News, accessed April 12, 2025, https://medcitynews.com/2024/12/transforming-patient-care-the-role-of-ai-powered-assistants/
What Steps Are Needed To Ensure Equitable Access to AI-Powered, accessed April 12, 2025, https://sustainability-directory.com/question/what-steps-are-needed-to-ensure-equitable-access-to-ai-powered-healthcare/
Priorities for an AI in health care strategy | The Health Foundation, accessed April 12, 2025, https://www.health.org.uk/reports-and-analysis/briefings/priorities-for-an-ai-in-health-care-strategy
Bias recognition and mitigation strategies in artificial intelligence healthcare applications - PMC - PubMed Central, accessed April 12, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11897215/
WHO launches global report on AI and health, identifying guiding principles to maximise the benefits of AI | Alzheimer Europe, accessed April 12, 2025, https://www.alzheimer-europe.org/news/who-launches-global-report-ai-and-health-identifying-guiding-principles-maximise-benefits-ai?language_content_entity=en
Population Health and Artificial Intelligence - PMC, accessed April 12, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11269274/
World Health Organization (WHO) - AI for Good - ITU, accessed April 12, 2025, https://aiforgood.itu.int/about-us/un-ai-actions/who/
AI's ability to transform value-based care | Healthcare Finance News, accessed April 12, 2025, https://www.healthcarefinancenews.com/news/ais-ability-transform-value-based-care
The VBC Newsstand weekly newsletter - VBCExhibitHall Library, accessed April 12, 2025, https://library.vbcexhibithall.com/aco-newsstand/
WHO issues first global report on Artificial Intelligence (AI) in health and six guiding principles for its design and use, accessed April 12, 2025, https://www.who.int/news/item/28-06-2021-who-issues-first-global-report-on-ai-in-health-and-six-guiding-principles-for-its-design-and-use
Publication: The Worldwide Governance Indicators: Methodology and 2024 Update - Open Knowledge Repository, accessed April 12, 2025, https://openknowledge.worldbank.org/entities/publication/4649907e-8902-4e74-a7ed-0e205e5e7919
State-of-the-Art Fast Healthcare Interoperability Resources (FHIR)–Based Data Model and Structure Implementations: Systematic Scoping Review - JMIR Medical Informatics, accessed April 12, 2025, https://medinform.jmir.org/2024/1/e58445
Methodology: How We Compiled the 2024 World Index of Healthcare Innovation - FREOPP, accessed April 12, 2025, https://freopp.org/whitepapers/methodology-how-we-compiled-the-2024-world-index-of-healthcare-innovation/
What Statistics Indicate Ai Adoption Rate in Healthcare? → Question, accessed April 12, 2025, https://sustainability-directory.com/question/what-statistics-indicate-ai-adoption-rate-in-healthcare/
Global FHIR Adoption Statistics: A Comprehensive Overview - Co-Desion, accessed April 12, 2025, https://codesion.com/global-fhir-adoption-statistics-a-comprehensive-overview/
4 Reasons Why the Adoption of FHIR Brings Immense Value to Medical Record Requesters, accessed April 12, 2025, https://mrocorp.com/blog/4-reasons-why-the-adoption-of-fhir-brings-immense-value-to-medical-record-requesters/
Broadband statistics - OECD, accessed April 12, 2025, https://www.oecd.org/en/topics/broadband-statistics.html
OECD broadband statistics update, accessed April 12, 2025, https://www.oecd.org/en/about/news/press-releases/2024/03/broadband-statistics-update.html
AI can support value-based care, but challenges must be addressed, accessed April 12, 2025, https://www.ama-assn.org/practice-management/digital/ai-can-support-value-based-care-challenges-must-be-addressed
Global Cyber Security Index, 2024 - Sanskriti IAS, accessed April 12, 2025, https://www.sanskritiias.com/current-affairs/global-cyber-security-index-2024
ITU Global Cybersecurity Index (GCI) | Indicator Profile | Prosperity Data360 - World Bank, accessed April 12, 2025, https://prosperitydata360.worldbank.org/en/indicator/WB+GTMI+I+43
Global Cybersecurity Index (GCI) 2024 - Drishti IAS, accessed April 12, 2025, https://www.drishtiias.com/daily-updates/daily-news-analysis/global-cybersecurity-index-gci-2024
Global Cybersecurity Index 2024 - AKSK, accessed April 12, 2025, https://aksk.gov.al/wp-content/uploads/2024/09/DOC-20240912-WA0002_240912_170509.pdf
Global Data Privacy Laws by Country (Updated October 2024) - GetTerms, accessed April 12, 2025, https://getterms.io/blog/global-data-privacy-laws-by-country
Data protection and privacy laws now in effect in 144 countries - IAPP, accessed April 12, 2025, https://iapp.org/news/a/data-protection-and-privacy-laws-now-in-effect-in-144-countries
The Worldwide Governance Indicators : Methodology and 2024 Update (English), accessed April 12, 2025, https://documents.worldbank.org/en/publication/documents-reports/documentdetail/099005210162424110
The Global Governance Index - SolAbility, accessed April 12, 2025, https://solability.com/the-global-sustainable-competitiveness-index/governance-capital
Regulatory Quality: Percentile Rank - World Bank Open Data, accessed April 12, 2025, https://data.worldbank.org/indicator/RQ.PER.RNK
The Role of AI Across US Health Care Payment Models, accessed April 12, 2025, https://www.insighthealth.ai/blog/role-of-ai-healthcare-payment-models
Payment Reform for Better Value and Medical Innovation - NAM, accessed April 12, 2025, https://nam.edu/perspectives/payment-reform-for-better-value-and-medical-innovation/
Practical Solutions |Artificial Intelligence and Payment - ASGE, accessed April 12, 2025, https://www.asge.org/home/resources/publications/practical-solutions/practical-solutions---artificial-intelligence-and-payment
Center for Program Integrity Request for Information on Using Advanced Technology in Program Integrity - CMS, accessed April 12, 2025, https://www.cms.gov/about-cms/components/cpi/downloads/center-for-program-integrity-advanced-technology-rfi.pdf
CMS' Value-Based Programs, accessed April 12, 2025, https://www.cms.gov/medicare/quality/value-based-programs
What is Value-Based Care? Glossary, Examples & More - OT Potential, accessed April 12, 2025, https://otpotential.com/blog/what-is-value-based-care
Value-Based Care: What It Is, and Why It's Needed | Commonwealth Fund, accessed April 12, 2025, https://www.commonwealthfund.org/publications/explainer/2023/feb/value-based-care-what-it-is-why-its-needed
ICT Development Index by Country 2025 - World Population Review, accessed April 12, 2025, https://worldpopulationreview.com/country-rankings/ict-development-index-by-country
Estonia is at the top of the United Nations e-government ranking, accessed April 12, 2025, https://e-estonia.com/estonia-is-at-the-top-of-the-un-e-government-ranking/
UK rises, and Denmark leads, in 2024 UN e-government rankings, accessed April 12, 2025, https://www.government-transformation.com/en/citizen-experience/uk-rises-and-denmark-leads-in-2024-un-e-government-rankings
Global Digitalization Index(GDI) 2024 - Huawei, accessed April 12, 2025, https://www.huawei.com/en/gdi
World Digital Competitiveness Ranking 2024 - IMD business school for management and leadership courses, accessed April 12, 2025, https://www.imd.org/centers/wcc/world-competitiveness-center/rankings/world-digital-competitiveness-ranking/
USA Today Men's Top 25 Poll - AP News, accessed April 12, 2025, https://apnews.com/6d6dc1e8e4c97ea0536bb3099338d861
World Talent Ranking 2024 - IMD business school for management and leadership courses, accessed April 12, 2025, https://www.imd.org/centers/wcc/world-competitiveness-center/rankings/world-talent-ranking/
What's the secret to Switzerland's status as a global talent hub? | World Economic Forum, accessed April 12, 2025, https://www.weforum.org/stories/2024/03/whats-the-secret-to-switzerlands-status-as-a-global-talent-hub/
The Essential List Of Future Skills Employers Will Be Looking For In 2030, accessed April 12, 2025, https://www.businessbecause.com/news/in-the-news/9647/essential-list-of-future-skills
The Global Talent Competitiveness Index, accessed April 12, 2025, https://www.fm-house.com/wp-content/uploads/2020/11/The-Global-Talent-Competitiveness-Index.pdf
The Global AI Index 2024: Overall and Sub Pillars Rank - Voronoi, accessed April 12, 2025, https://www.voronoiapp.com/technology/The-Global-AI-Index-2024-Overall-and-Sub-Pillars-Rank-4166
F acts igures - CPBRD, accessed April 12, 2025, https://cpbrd.congress.gov.ph/wp-content/uploads/2025/02/FF2025-01-Global-AI-Index.pdf
Saudi Arabia Earns Top Marks in Global AI Index for National Strategy - وكالة الأنباء السعودية, accessed April 12, 2025, https://spa.gov.sa/N2085216
For The Second Consecutive Time Saudi Arabia Ranks 2nd Among G20 Countries in the ITU's ICT Development Index 2024, accessed April 12, 2025, https://cst.gov.sa/sl/l16
ICT Development Index - Wikipedia, accessed April 12, 2025, https://en.wikipedia.org/wiki/ICT_Development_Index
networkreadinessindex.org, accessed April 12, 2025, https://networkreadinessindex.org/#:~:text=According%20to%20the%202024%20Network,most%20network%2Dready%20societies%20globally.
2024 Network Readiness Index: USA, Singapore, and Finland lead the way for third consecutive year - Tech Wire Asia, accessed April 12, 2025, https://techwireasia.com/2024/11/usa-singapore-and-finland-lead-global-network-readiness-rankings-for-2024/
IMD World Digital Competitiveness Ranking 2024 - CEDA, accessed April 12, 2025, https://www.ceda.com.au/researchandpolicies/research/economy/imd-world-digital-competitiveness-ranking-2024
Data Center, accessed April 12, 2025, https://publicadministration.un.org/egovkb/en-us/data-center
Regulatory Quality: Percentile Rank | Indicator Profile | Prosperity Data360 - World Bank, accessed April 12, 2025, https://prosperitydata360.worldbank.org/en/indicator/WB+WWGI+RQ+PER+RNK
ITU publishes 2024 Global Cybersecurity Index list - CERT.RS, accessed April 12, 2025, https://www.cert.rs/en/vest/1276-ITU-objavila-globalnu-listu-indeksa-informacione-bezbednosti-za-2024-godinu.html
From Role Models to Evolving Players: Assessing Arab States in the ITU's GCI 2024, accessed April 12, 2025, https://www.telecomreview.com/articles/reports-and-coverage/8392-from-role-models-to-evolving-players-assessing-arab-states-in-the-itu-s-gci-2024
Global Talent Competitiveness Index by INSEAD, accessed April 12, 2025, https://fcsc.gov.ae/en-us/Pages/Competitiveness/Reports/Global-Talent-Competitiveness-Index.aspx?rid=27
World's most talent competitive countries, ranked for 2023 - The World Economic Forum, accessed April 12, 2025, https://www.weforum.org/stories/2023/11/most-talent-competitive-countries-2023/
The Global Talent Competitiveness Index 2023: What a Difference Ten Years Make and What to Expect for the Next Decade | Singapore EDB, accessed April 12, 2025, https://www.edb.gov.sg/en/business-insights/market-and-industry-reports/the-global-talent-competitiveness-index-2023-what-a-difference-ten-years-make-and-what-to-expect-for-the-next-decade.html
Mirror, Mirror 2024: A Portrait of the Failing U.S. Health System - Commonwealth Fund, accessed April 12, 2025, https://www.commonwealthfund.org/publications/fund-reports/2024/sep/mirror-mirror-2024
Mirror, Mirror 2024: A Portrait of the Failing U.S. Health System – Comparing Performance in 10 Nations - Commonwealth Fund, accessed April 12, 2025, https://www.commonwealthfund.org/sites/default/files/2024-09/Blumenthal_mirror_mirror_2024_final_v2.pdf
Mirror, Mirror 2021: Reflecting Poorly - Commonwealth Fund, accessed April 12, 2025, https://www.commonwealthfund.org/publications/fund-reports/2021/aug/mirror-mirror-2021-reflecting-poorly
Commonwealth Fund “Mirror, Mirror 2024: A Portrait of the Failing U.S. Health System” Shows How Much Of A Healthcare Outlier America Really Is, accessed April 12, 2025, https://www.healthcarelabyrinth.com/commonwealth-fund-mirror-mirror-2024-a-portrait-of-the-failing-u-s-health-system-shows-how-much-of-a-healthcare-outlier-america-really-is/
Global Initiative on AI for Health, accessed April 12, 2025, https://www.who.int/initiatives/global-initiative-on-ai-for-health



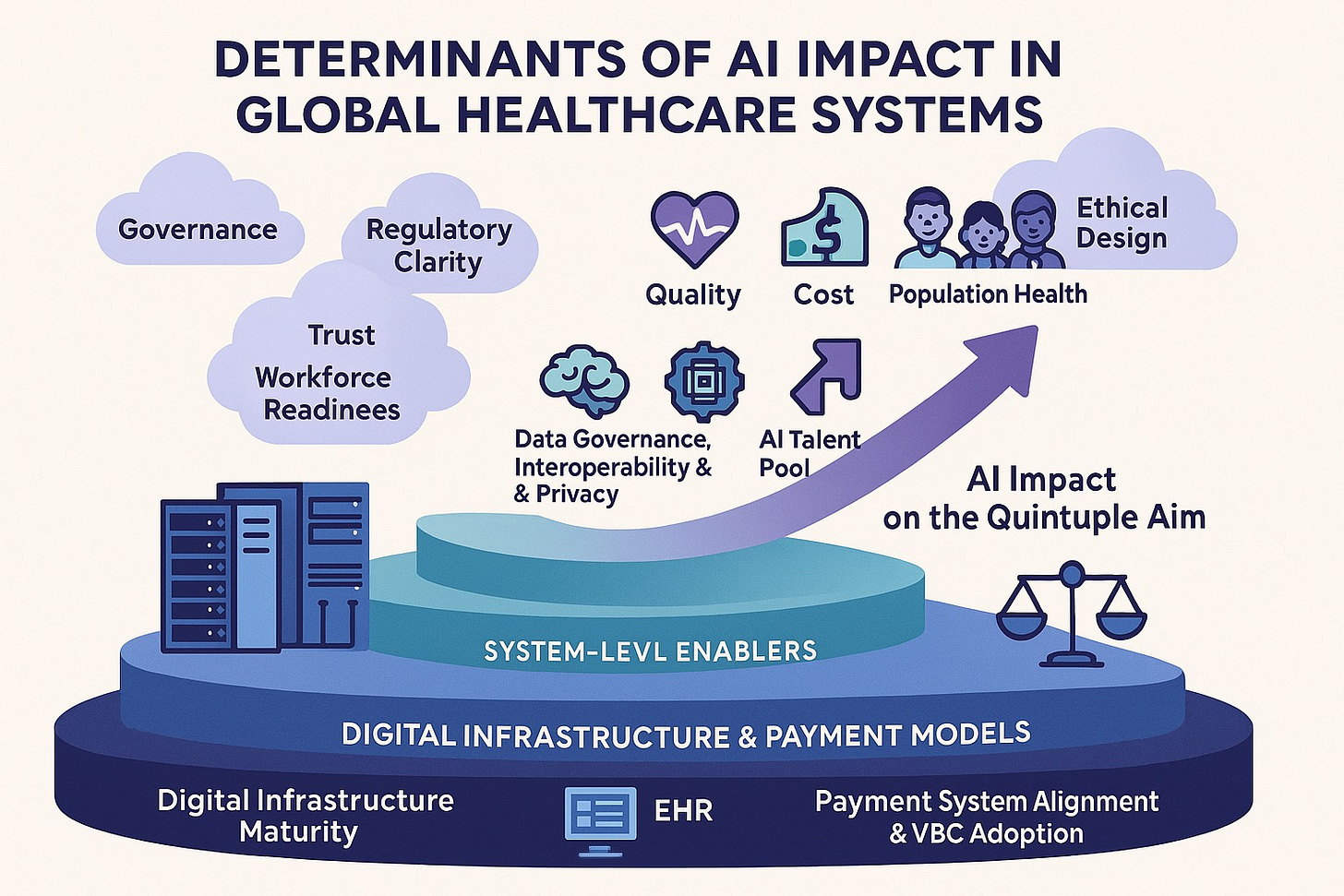
After reading it, all I can say is that for AI to improve healthcare, it is not just about the tech. It also depends on whether the system and the people are ready. Data and equipment alone are not enough. If the mindset and regulations do not keep up, AI cannot make much of a difference. This article does cover things quite comprehensively, but when it comes to real implementation, it all comes down to execution